- Remote patient monitoring. Definition and technology growth factors
- Power of remote patient monitoring technology: an example
- How does remote patient monitoring work
- Types of remote patient monitoring in existence
- Engineering in remote patient monitoring. Guidelines and challenges
- Specific guidelines of RMP implementation
- 3 special challenges for any RMP implementation guidelines
- Choose Andersen as your technology partner
These remote patient monitoring guidelines provided by Andersen are based both on our constant monitoring of this expanding technology and the successful track-record of the multiple, highly-functional, and totally compliant projects we have implemented. As such, it combines our theoretical and practical understanding of the industry.
We would like to kick off the discussion by citing an obvious trend. The demand for remote patient monitoring, as a segment of the telemedicine market, is increasing, quantitatively and qualitatively. In 2021, this particular sector held a value of $1.9 billion. Fast forward to 2031, and experts anticipate its valuation to soar to $8.5 billion. The allure of this technology has led to substantial investments from both privately-owned and state-operated healthcare entities.
Consider this figure, for instance: per a 2019 report from the US-based Consumer Technology Association, nearly 90% of healthcare providers had either already put money into or were contemplating investments in remote medical technology. It is an integral element of their organizational guidelines. This strategic move is motivated by a myriad of tangible advantages and pressing issues.
Remote patient monitoring. Definition and technology growth factors
The Encyclopedia of Health Economics gives us the following guidelines. Any remote patient monitoring system is specifically designed to record patients’ ‘biometric data’ and transfer it to a ‘central monitoring facility’ for subsequent interpretation. As such, the whole sphere of remote patient monitoring technology can be conceptualized as a sub-branch of a bigger telehealth market, intended to provide remote care.
Mainly, three factors are at play here, supporting investments in remote patient monitoring software development:
- The global population is aging steadily. This hard factor defines not only separate guidelines, but also the global policy framework. As the World Health Organization reminds us, around 2030, every sixth individual will be 60 years old or over. Simultaneously with this, the prevalence rates of various persisting conditions are also inevitably on the rise.
What makes the issue even more topical is that many of those aging potential patients will have low-and-middle incomes, with some serious disbalances in their respective national healthcare systems. Affordable and accessible remote tracking technology promises to address this challenge, to some extent at least;
- Concurrently with this first trend, healthcare spending is growing. It is now below its record high during the COVID-19 wave, but hasn’t returned to the pre-crisis level. For instance, as the OECD says, the ratio of health expenditure to GDP, within that group, has decreased from its highest point of 9.7% during the peak of the crisis back in 2021 to 9.2% in 2022.
Despite this decline, the proportion of GDP allocated to health still surpasses the pre-pandemic level of 8.8%. Ways are needed to mitigate this growing expenditure, while still being able to achieve results, i.e. help people successfully. Remote observation technology could make that spending more effective;
- Interestingly, in spite of the fact that governments allocate more and more funds to healthcare, significant portions of the global population are still underserved. As the WHO stresses, roughly half of the planet’s population lacks access to crucial health services. This observation holds true not only when developing countries are involved.
Some of the most advanced and prosperous economies are facing similar problems, e.g. the US (3.6 million people in America lack access to care, as the facilities are located too far from them) or the UK (approximately one-third of adults in England don’t believe they’re able to access prompt healthcare services because of their locations). Here, remote patient monitoring technology might also have a prominent part to play.
Having examined the remote patient monitoring definition-specific questions, let’s quickly assess its empirically measurable pros.
Power of remote patient monitoring technology: an example
Guidelines shaped in the RPM domain are defined by the better results it generates. Design and development efforts must be focused on maximizing those benefits, which are, from doctors’ perspectives, as follows (the figures we cite below are taken from the same report by the US Consumer Technology Association we have already referred to):
- Improved patient outcomes in 49% of cases. This is totally comprehensible, as the more dependable information medical professionals are able to obtain and the more seamless the data exchange technology is in real-time, the better decisions they make;
- Higher treatment adherence and compliance rates in 44% of cases. As long as people are aware of the fact they are constantly tracked, they will be more likely to follow doctors’ prescriptions and advice;
- With an RPM system monitoring their health indicators continuously, remote patients are more inclined to treat their own health issues earnestly. Indeed, “increased ownership over their health” was reported in 42% of cases.
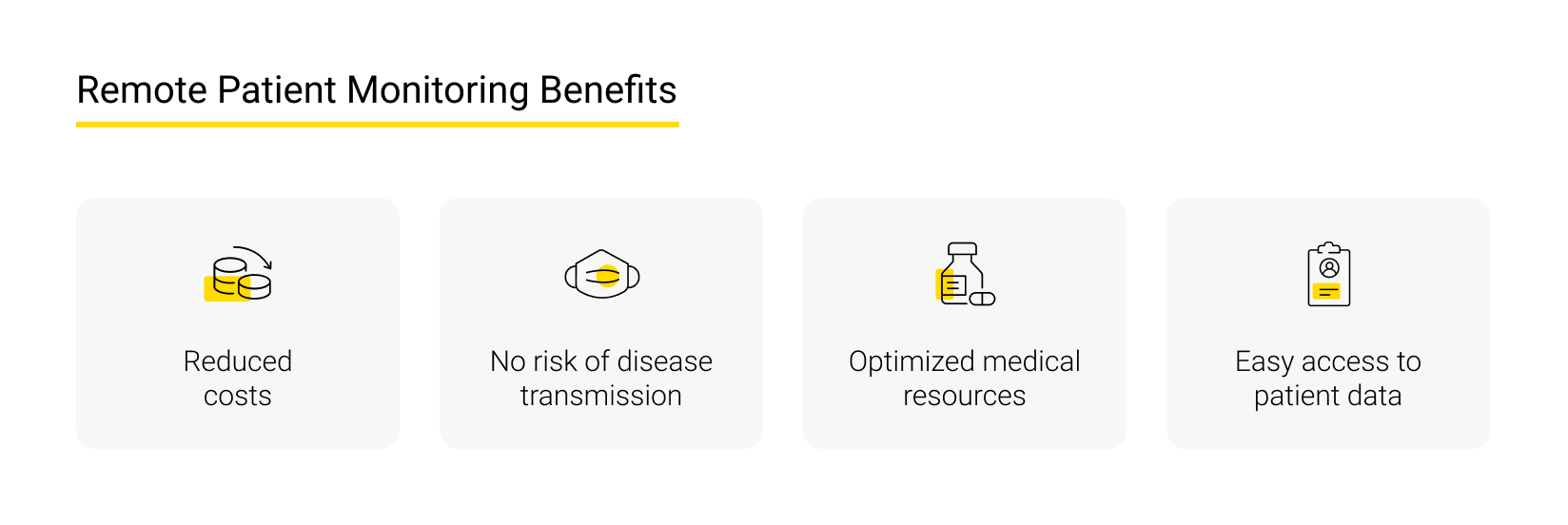
When it comes patients’ attitudes (in the light of technology guidelines stemming from them), the three crucial benefits are:
- First, people are delighted to enjoy a chance to receive exhaustive info concerning personalized medical care (43%);
- Second, they are happy to be in the right position to get “faster access to health care services” (42%);
- Finally, with the potential of the remote monitoring systems unleashed, they feel they can exert extra control “over their own well-being” (37%). This sense of newly found agency must be a great psychological bonus.
How does remote patient monitoring work
Opinions expressed by both parties in the section above dictate this set of guidelines: an RPM system is to:
- Acquire info smoothly, incessantly, and precisely;
- Process and store it safely;
- Ensure the information itself is easily readable.
In line with that, the answer to this question in your unique situation, “How does remote patient monitoring work,” must cover these four RPM dimensions:
- A data acquisition system is required. It is to build upon “different sensors or devices with embedded sensors” capable of transmitting data wirelessly. Their mission is to track and record information and continuously forward it;
- As for the data processing part, it can be defined as a “system with data receiving and transmitting capability and a processing unit”;
- On top of that, end-terminals used by medical professionals must be in place. For instance, doctors can use PCs installed at their hospital, smartphones, tablets, or any other dedicated devices and databases. If your remote monitoring guidelines imply that patients can be informed, some point of entry must be granted to them;
- Finally, a communication network responsible for uniting all these elements within a single framework is a must.
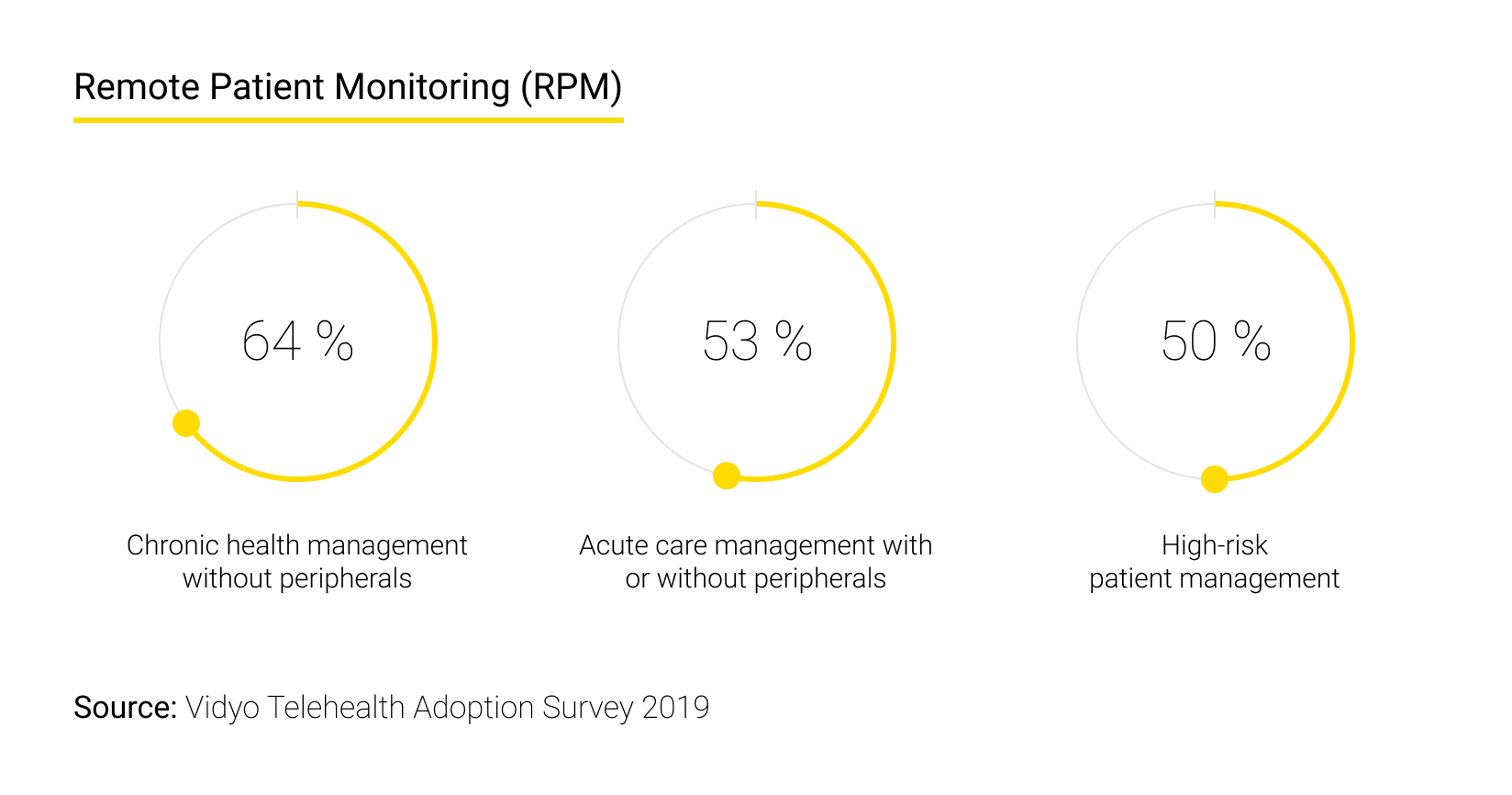
Types of remote patient monitoring in existence
As previously noted, the utilization rates of remote monitoring devices are skyrocketing. In 2020 for instance, 29 million individuals in the US alone were using these devices, a number projected to surpass 70 million by 2025, per Insider Intelligence.
This growth is not solely attributed to an increase in aging or unhealthy individuals who could benefit from existing monitoring devices. The expanding popularity is also a result of the decreasing cost and enhanced affordability of current monitoring devices, coupled with the continuous emergence of new and advanced types.
Telehealth.hhs.gov, an official government-run information hub, highlights specific RPM devices that are currently experiencing significant demand. That list of types of remote patient monitoring options is as follows:
- Scales for gauging body weight, invaluable given the prevalence of obesity;
- Pulse oximeters utilized to check both pulse rates and blood oxygen saturation levels (an especially crucial function against the backdrop of the ongoing COVID-19 pandemic);
- Blood glucose meters, functioning as indispensable tools for monitoring and controlling blood sugar levels, which is a critical factor for many individuals with diabetes, a full-fledged daily matter of life and death;
- Blood pressure monitors, which are a priceless assistant for the elderly and other vulnerable groups;
- Apnea monitors are used to evaluate the respiratory and cardiac rates of infants once they are discharged from hospitals;
- Heart monitors employed to monitor individuals with heart conditions, facilitating prompt intervention and necessary timely measures;
- Tailored monitors designed for individuals suffering from dementia and Parkinson's disease, essential to offer support for those dealing with mental health challenges;
- Breathing apparatuses providing breathable air in an adjustable way;
- Fetal monitors required to track the growth of fetuses for successful eventual delivery.
Engineering in remote patient monitoring. Guidelines and challenges
Healthcare is a sensitive and heavily regulated domain. That is self-evident, as the price of a mistake is unbelievably high. Human lives must be saved, privacy issues are to be observed, corporate quality standards should be followed, and of course countless laws and protocols have to be applied. It mandates a wide set of special implementation guidelines.
Specific guidelines of RMP implementation
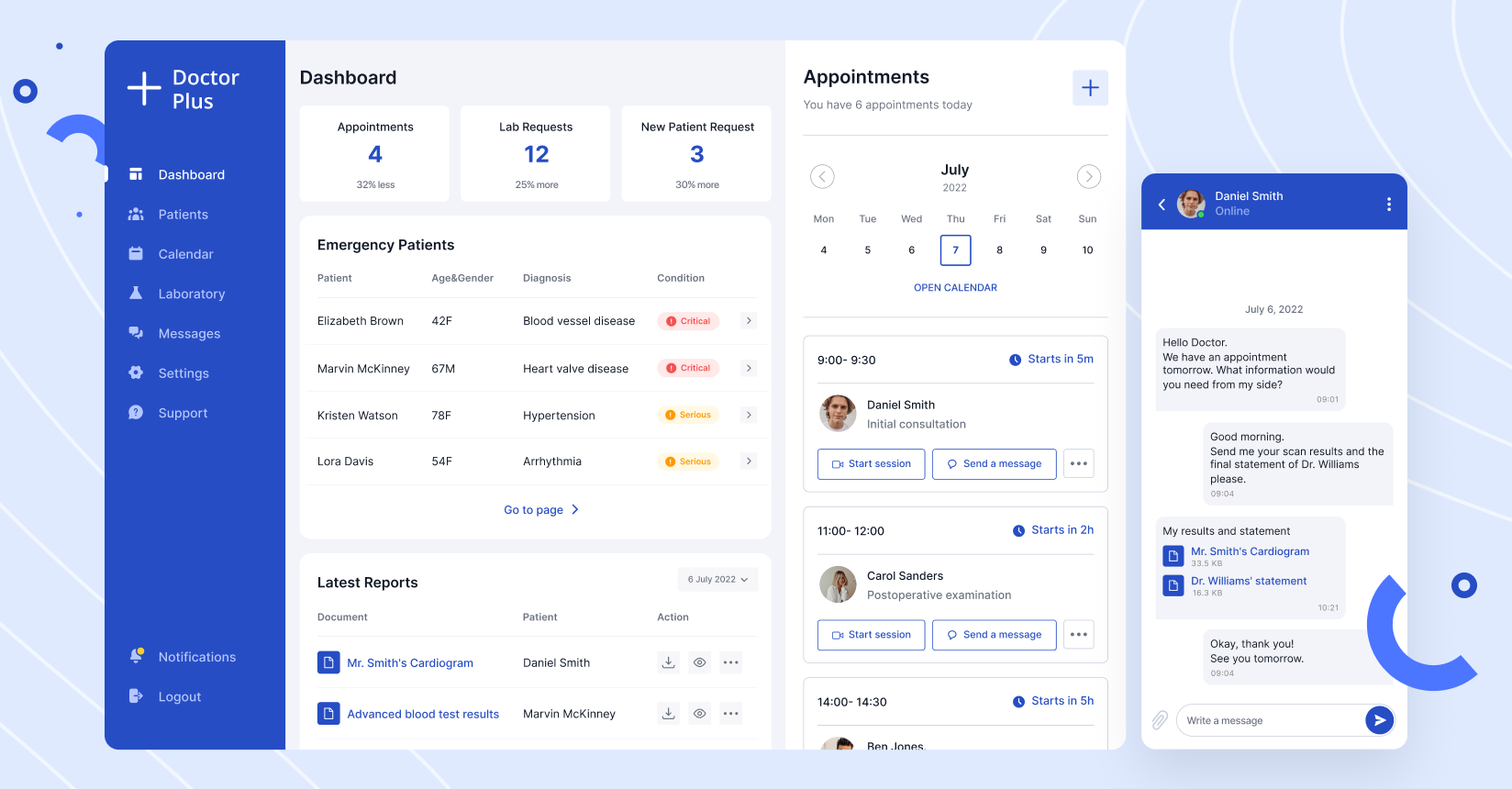
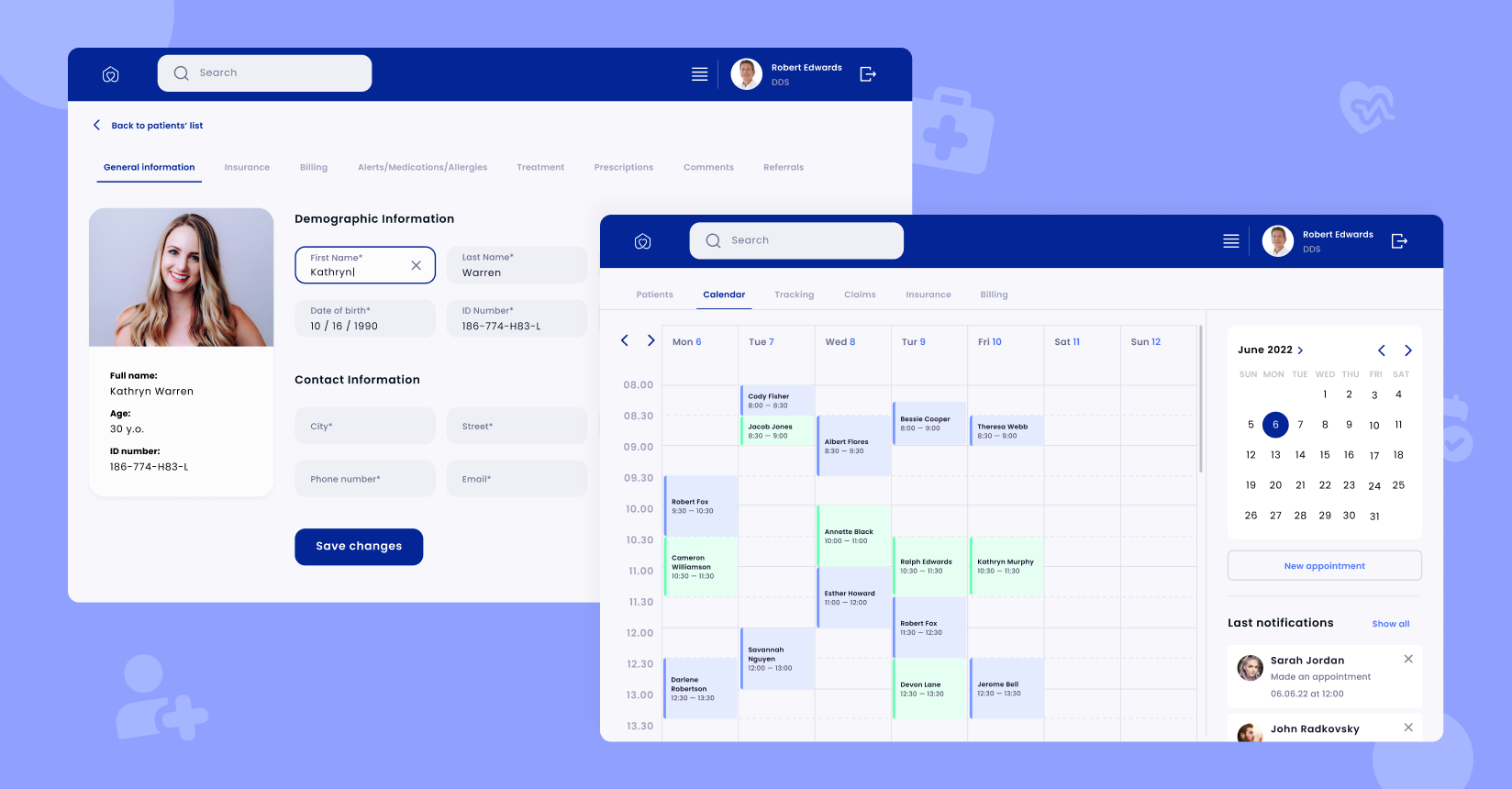
- Seamless integration with in-house EMR/EHR systems holds paramount importance. The remote patient monitoring capabilities you are considering should align perfectly with the system used for storing the comprehensive historical data of your patients. This data must be stored for an extended duration, adhering strictly to relevant legislation and guidelines;
- Secondly, special emphasis must be placed on usability, intuitiveness, and friendliness. A significant portion of RPM users comprises elderly individuals who may not be familiar with modern technology intricacies. Furthermore, it's not uncommon for remote patients to experience varying degrees of mental incapacitation, whether temporary or permanent. Therefore, the “machinery” offered to your end-users should prioritize simplicity and ease of control. These UI/UX-related guidelines cannot be underestimated;
- Lastly, ensuring integration with billing solutions is essential. Remote payment considerations are integral when dealing with patients located far from the facility. Healthcare providers should establish a system to notify them about upcoming payments and billing updates, generate bills, make and process payments, and maintain comprehensive documentation. This ensures a smooth process for handling financial aspects related to proper monitoring practices, medical care, and business guidelines.
3 special challenges for any RMP implementation guidelines
While capitalizing on the benefits brought about by RPM, providers also need to tackle a range of vital challenges to put such systems in action fruitfully. Domain experts typically accentuate the following ones to consider while working on your technology guidelines:
Challenge #1 for your technology guidelines. In the realm of wearables, the challenge of battery life remains a potential impediment to progress. Despite recent technological advancements, the availability of energy remains finite, even though monitoring devices may now last longer on a single charge. This underscores the importance of crafting solutions for these devices that can efficiently employ functions such as 'standby, sleep, power save, hibernate, and shutdown' without compromising background efficiency. Take them all into consideration while working on your engineering guidelines.
Challenge #2 for your technology guidelines. Ensuring the security of data presents a clear and prominent priority among other guidelines. Medical confidentiality stands as the utmost priority within any information protection framework. This is doubly true when we discuss remoteness, connectivity, and other projects pertaining to the Internet of Things in healthcare. Addressing this monitoring challenge requires full adherence to the HIPAA-, PIPEDA-, GDPR-standards, or other norms dominating your jurisdiction.
Challenge #3 for your technology guidelines. Protected and impeccable integration with third-party cloud vendors. As MachineDesign’s experts stress, “uploading patient data directly to the cloud can save space.” Cooperating with endorsed cloud experts assists with risk mitigation in this context.
Choose Andersen as your technology partner
In the capacity of a technology partner, Andersen is fully prepared to equip you with remote monitoring capabilities. Our talent pool of 300 healthcare-focused engineers and our 150+ implemented projects guarantee that we can assume responsibility for your monitoring technology endeavors in their entirety, including:
- Usability guidelines;
- Data safety guidelines;
- IoT-specific guidelines;
- Cloud-specific guidelines,
- ML-related guidelines (as we firmly believe in AI and the future of healthcare as a data-driven intelligent domain, Andersen’s team can help not only with data readings, transfers, and storage, but also with advanced assisting algorithms for info interpretation).
Feel free to contact us and initiate the discussion of your remote monitoring needs!